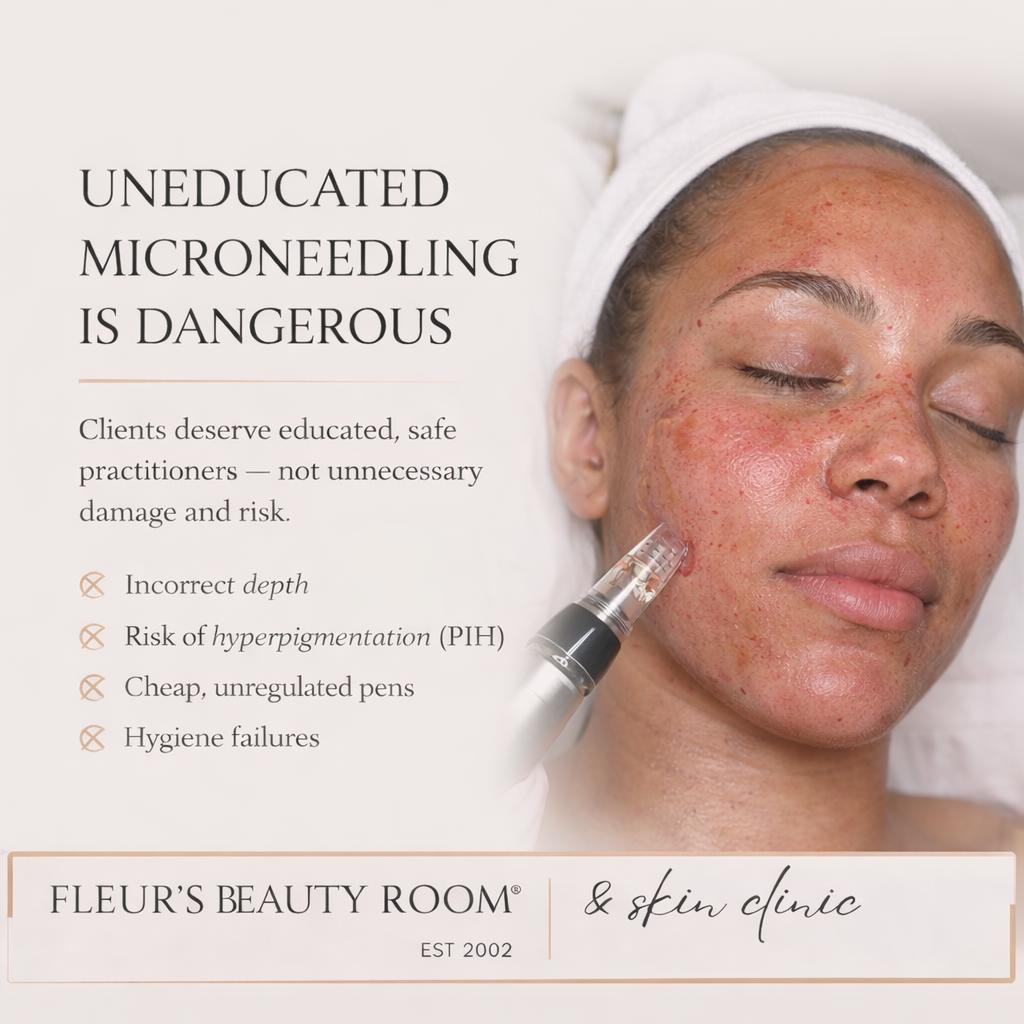
Client safety comes first
Microneedling is a highly effective treatment when performed correctly and with a clear understanding of skin anatomy.
However, problems can arise when techniques are overly aggressive, practitioners lack proper anatomical education, or hygiene standards are compromised.
This article explains what can go wrong with microneedling — and how clients can protect their skin by knowing what to look for before treatment.
I’ve recently seen microneedling content online that looks extremely aggressive — heavy redness, visible trauma and forceful techniques — and I want to share why this genuinely concerns me from a client safety and education perspective.
More damage does not equal better results.
✔️ Depth & skin anatomy matter
Effective cosmetic microneedling works at the epidermal–dermal junction. This is where controlled micro-injury signals collagen production withoutexcessive inflammation.
Going too deep increases pain, healing time, and complications — while actually reducing treatment effectiveness.
✔️ Post-inflammatory hyperpigmentation (PIH) risk
Over-traumatising the skin significantly increases the risk of PIH, especially for:
• Melanin-rich skin tones
• Clients with hormonal or existing pigmentation
• Clients prone to inflammation
Excessive redness and trauma are not harmless — inflammation is one of the biggest triggers for long-term pigmentation issues.
✔️ Cheap pens are a growing industry issue
There are many low-cost, poorly manufactured microneedling penscirculating in the industry. These often have:
• Inconsistent or inaccurate needle depth
• Poor needle stability
• Increased vibration and skin drag
• Blunt or poorly manufactured needles
This leads to unnecessary pain, tearing of the skin and unpredictable outcomes.
✔️ Hygiene is non-negotiable
Safe microneedling requires:
• Sterile, single-use cartridges
• Barrier sleeves on the pen device
• Strict infection-control protocols
Without these, the risk of cross-contamination and infection increases significantly.
⸻
What worries me most
Out of genuine concern, I contacted the training academy behind some of this content and asked a very basic question:
Did they know what the epidermal–dermal junction is, and where it sits within the skin?
They did not.
This is deeply worrying — not just because of one treatment, but because these are people actively training others, who are then released to work on members of the general public.
⸻
What this means for clients
When practitioners are uneducated or incorrectly educated, clients may experience:
• Excessive pain and prolonged healing
• Increased risk of PIH and pigmentation issues
• Compromised skin barrier function
• Infection or cross-contamination risks
• Long-term texture damage or scarring
Clients trust practitioners with their skin. That trust depends on anatomy knowledge, proper training, quality equipment and ethical practice — not dramatic visuals for social media.
Red, inflamed skin may look “advanced” online, but true results come from precision, education and respect for the skin.
⸻
Please ask questions before treatment 🤍
• What depth are you working at and why?
• How do you minimise inflammation and PIH risk?
• What device are you using and how is it hygienically protected?
• What training and anatomical education do you have?
Education protects skin — and clients deserve nothing less.